Palliative care meaning explained: What is it and how can it help?
Learn the meaning of palliative care, who it is for, what it includes, and how to access this type of support when you have a serious illness.
Author: Sensible Care

Palliative care is specialised support for people with serious or life-limiting illnesses. It focuses on comfort, symptom relief, and emotional, practical, and spiritual support for both the person and their family. In Australia, it's based on need rather than time left and can be accessed through the Support at Home program.
Palliative care is a form of specialised, person- and family-centred care.
It's for people with an active, progressive, advanced, or life-limiting illness. This means the illness is ongoing and serious, and it's expected to get worse over time.
The main purpose of palliative care is to improve quality of life and relieve pain.
It looks at the whole person, not just their medical diagnosis. Care teams look at how the illness affects the body, emotions, relationships, and daily life.
Palliative care supports physical symptoms, emotional and psychosocial needs, and spiritual and practical concerns.
If you want to learn more about palliative care, this article will tell you everything you need to know.
What palliative care includes
Palliative care combines various types of support into one coordinated approach. The goal is to help people feel as comfortable, informed, and supported as possible.
This includes:
- Symptom management
- Psychosocial and emotional support
- Practical support
- Advanced care planning
- Coordination of care
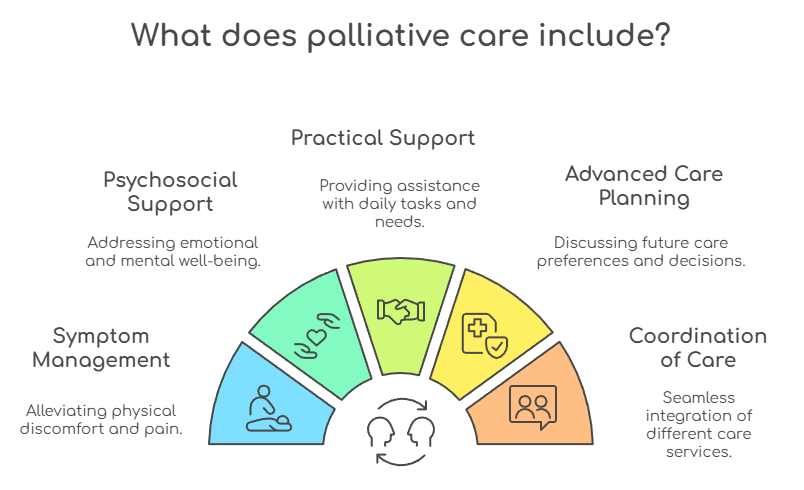
Symptom management
The first goal of palliative care is symptom management, which can include help with:
- Pain
- Breathlessness
- Nausea
- Fatigue
- Other distressing symptoms
These symptoms can make everyday tasks much harder. Palliative care teams work with the person and their doctor to adjust medications and other treatments so symptoms are easier to live with.
Psychosocial and emotional support
Psychosocial and emotional support is another key aspect of palliative care. It can include:
- Support for patients, families, and carers
- Counselling
- Bereavement support
Living with a serious illness can cause worry, fear, and stress for everyone involved. Emotional and psychosocial support gives people a safe space to talk, ask questions, and feel heard.
Practical support
Palliative care also includes practical support, which may involve:
- Equipment to help at home
- Home nursing
- Links to community services
These supports may help someone stay at home if that is their preference. Equipment and home nursing can make day-to-day care safer and more manageable for both the person and their carers.
Advance care planning
Palliative care may also involve advance care planning, which includes:
- Discussing treatment options and preferences
- Helping complete advance care directives and other legal documents
These discussions help people think about what matters most to them if their condition worsens. Writing these wishes down can guide future care and help families feel more confident in decision-making.
Coordination of care
Coordination of care in palliative care often means:
- Linking GPs, specialists, and community services
- Working with hospitals
- Working with residential aged-care facilities
Palliative care teams help everyone involved in the person's care stay on the same page. This can reduce confusion, repeated questions, and the stress of having to explain the situation many times.
Accessing palliative care
Accessing palliative care can feel overwhelming, especially when you're dealing with a serious illness.
The good news is that support is available in many settings, and you do not need to wait until the very end of life.
Understanding where to start and who to talk to can make it easier to get the right help at the right time.
Who can receive palliative care?
Palliative care is not limited to older people.
People of any age can receive it, including children with serious conditions. The focus is always on the person's needs, not their age (or life expectancy).
It's mainly for people with a life-limiting or serious chronic illness, such as:
- Cancer
- Heart failure
- Chronic obstructive pulmonary disease (COPD)
- Neurological conditions
- Some paediatric conditions
These illnesses can cause complex symptoms and ongoing stress. Palliative care helps manage these challenges over time, not just at the very end of life.
Someone may benefit from palliative care when:
- Symptoms are hard to manage
- Treatments are complex
- Extra emotional and practical support would help
A person does not have to be in the final days or weeks of life to receive palliative care. It can be helpful:
- Shortly after diagnosis
- During active treatment
- Later in the illness, if things become more complicated

Referral usually happens through a GP, specialist, or hospital team. These health professionals can recognise when palliative care might make a difference. They can then connect the person and their family with appropriate local services.
Where is palliative care delivered?
Palliative care can be provided in different settings. This flexibility helps people receive care in a place that feels most comfortable and practical for them and their family.
Common settings include at/in:
- Home, through palliative care teams or the Support at Home program
- Hospitals, via specialist palliative care consult teams or wards
- Hospices, which may be run by charities or health services
- Residential aged-care facilities
- Some outpatient and clinic settings

When care is provided at home, palliative care teams may visit to review symptoms, adjust medicines and support carers. Home care can be especially important for those who prefer familiar surroundings.
In hospitals, palliative care teams may see people on different wards. They help the primary care team manage symptoms, make choices, and plan for when patients leave the hospital.
Hospices offer more intensive palliative care in a dedicated setting. They're calm and supportive environments for people who need more complex care or cannot be at home.
In residential aged-care facilities, staff may work with palliative care teams. Together, they support residents with life-limiting and chronic illnesses.
Some people may also attend outpatient or clinic appointments. In these cases, they review their care plan and symptoms with a palliative care team and then return home.
How to access palliative care in Australia
The first step is usually to talk with your GP or treating specialist. You can ask them directly for a referral to local palliative care services if you feel extra support would help.
If you already receive in-home aged care, your provider under the Support at Home program may also help you understand your options and next steps.
Support may be available through:
- Public hospitals
- State and territory health services
- Community palliative care providers
- In-home aged care services funded through the Support at Home program
These services can offer assessment and ongoing care. An assessment helps the team understand your medical history, current symptoms, support network, and goals for care.
Following this, you and your carers create a plan together. This plan can change over time as your needs evolve.
You can also find services by checking your state or territory health department website and Palliative Care Australia. These websites can help you see what services exist in your region. They can also guide you on questions to ask your GP or specialist when discussing a referral.
Funding and typical costs
In Australia, many types of palliative care are publicly funded. This helps reduce the financial burden on people and families already dealing with a serious illness.
Palliative care in public hospitals and many community palliative care programs is largely funded by a mix of:
- Australian Government funding (including Medicare)
- State and territory governments
- Local health services

This means many core services are available at low or no direct cost in public settings.
Medicare helps subsidise:
- GP consultations
- Specialist consultations
The Pharmaceutical Benefits Scheme (PBS) helps subsidise many medicines used in palliative treatment. This can make important symptom-relief medicines more affordable.
Some private services or private hospice care may involve out-of-pocket costs. These costs can vary, so it is important to ask providers about fees early.
Charities and not-for-profit hospices may offer subsidised care. They often use donations and grants to lower costs for patients and families.
For eligible veterans, the Department of Veterans' Affairs (DVA) can provide coverage.
The National Disability Insurance Scheme (NDIS) may fund some supports for younger people with disability. However, general palliative care funding is usually provided through health services, not the NDIS.
For older people receiving palliative care at home, in-home aged care may be funded through the Australian Government's Support at Home program.
This support can sit alongside specialist palliative care, helping with daily tasks, personal care, and other services that make it easier to remain at home.
Palliative care through Support at Home
For many older people, palliative care is delivered at home.
Government-funded home care can help make this possible. It can support symptom management, personal care, and carers.
In the past, this was mainly done through Home Care Packages (HCPs). These packages had four levels and could fund these services:
- Nursing care and symptom management
- Personal care, such as showering and dressing
- Help with medications, meals, and daily tasks
- Equipment and home modifications
- Respite and support for carers
From 1 November 2025, the Australian Government's new Support at Home program replaced Home Care Packages.
Support at Home is designed to simplify and improve in-home aged care. It still aims to help older Australians live safely and independently at home for as long as possible.
For someone receiving palliative care at home, Support at Home funding can help with:
- Regular nursing visits and symptom monitoring
- Personal care when mobility or strength declines
- Equipment and minor home changes to improve comfort and safety
- Respite and practical help for family carers
End-of-Life Pathway
A key feature of palliative care is the End-of-Life Pathway. This is a short-term, higher-level support option for older people who:
- Have been diagnosed with three months or less to live
- Wish to remain at home during this time
The End-of-Life Pathway provides extra funding for in-home aged care services. It offers a budget of $25,000 over 12 weeks (usable for up to 16 weeks) to increase support at home.
Services may include:
- Nursing and other clinical supports
- Personal care, such as showering and toileting
- Help around the home and respite care
- Care management and coordination with palliative care teams
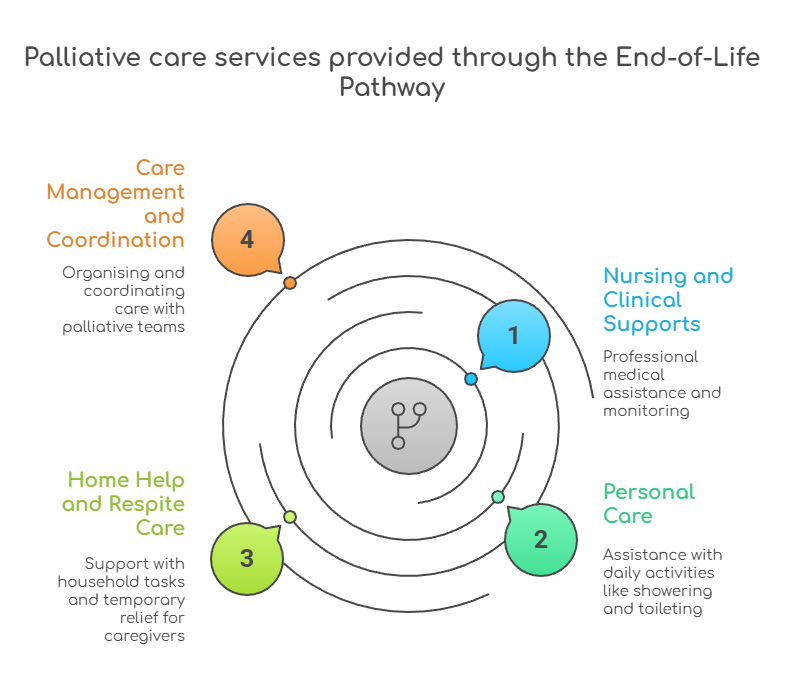
This pathway works alongside government-funded palliative care services; it does not replace them. It helps people receive both specialist palliative care and extra home care support at the same time.
Access usually starts with My Aged Care and an aged care assessment. A GP or nurse practitioner must complete a special End-of-Life Pathway form to confirm eligibility.
If you already receive home care through Support at Home, your provider can help request a review and transition you onto the End-of-Life Pathway.
Bringing palliative care together
Palliative care brings medical, emotional, and practical support into one coordinated approach.
It is there for people of all ages living with serious or life-limiting illnesses. Care is based on what you need, not just how long you may have left.
If you or someone you love is facing a serious illness, you do not have to manage it alone. Talking with your GP, specialist, or local palliative care team is a strong first step.
Sensible Care is here to help you understand your options and plan the next steps.
If you would like more information about palliative care and Support at Home, contact Sensible Care to discuss your situation. Together, we can explore what kind of care might be right for you and your family.
Take the Next Step in Care
Download our Info Kit or speak to one of our friendly team members today.
Need Help Getting Started?
Reach out on your terms, pick a time that suits you and let’s talk about how we can help.
.webp)
.svg)


