Sundowning in dementia explained: What is it and how to manage it?
Learn what sundowning is, why it happens to people with dementia, and practical tips to manage it safely at home with Sensible Care.
Author: Sensible Care

Sundowning is a common dementia-related phenomenon. It happens when the dementia patient becomes more confused or upset, often in the late afternoon or evening. Common triggers include fatigue, fading light and shadows, overstimulation, or unmet needs like hunger, pain, or needing the toilet. A consistent routine, better lighting, calmer evenings, and comfort checks can reduce this type of behaviour.
If you're caring for someone with dementia who becomes more confused, agitated, or restless later in the day, what you're seeing is sundowning.
This common pattern affects many people living with dementia at some point. It can be one of the most challenging aspects of dementia care for families and carers alike.
This guide explains what sundowning is, why it happens, common signs and triggers, and what you can do about it. We'll also talk about how Support at Home in-home care can help safely manage sundowning behaviour.
What is sundowning?
Sundowning is a pattern of behaviour changes that usually worsen in the late afternoon, evening, or early night. It's a common symptom of dementia.
According to Dementia Australia, people experiencing sundowning may become more confused, anxious, or restless during these hours.
Sundowning and dementia often go together, but it's not a separate diagnosis.
It's a behaviour pattern that can happen in different forms of dementia. Symptoms can vary significantly between individuals and dementia stages.
The term comes from the timing of these symptoms, which tend to emerge around sunset and continue into the night. That being said, some people may experience them earlier in the afternoon.
Recognising sundowning symptoms
Sundowning behaviour can look different from person to person, and can change over time. Common signs include:
- Increased confusion or disorientation – not knowing the time, place, or recognising familiar people
- Restlessness – pacing, fidgeting, or an inability to settle
- Mood changes – anxiety, frustration, aggression, crying, or paranoia
- Agitation – becoming upset, demanding, or refusing care
- Heightened sensitivity – reacting strongly to noise, lights, or shadows
- Suspicion or hallucinations – particularly in low light, seeing or hearing things that aren't there
- Sleep disturbances – difficulty falling asleep or confusing day and night
- Shadowing behaviour – following carers around or repeatedly asking to "go home"
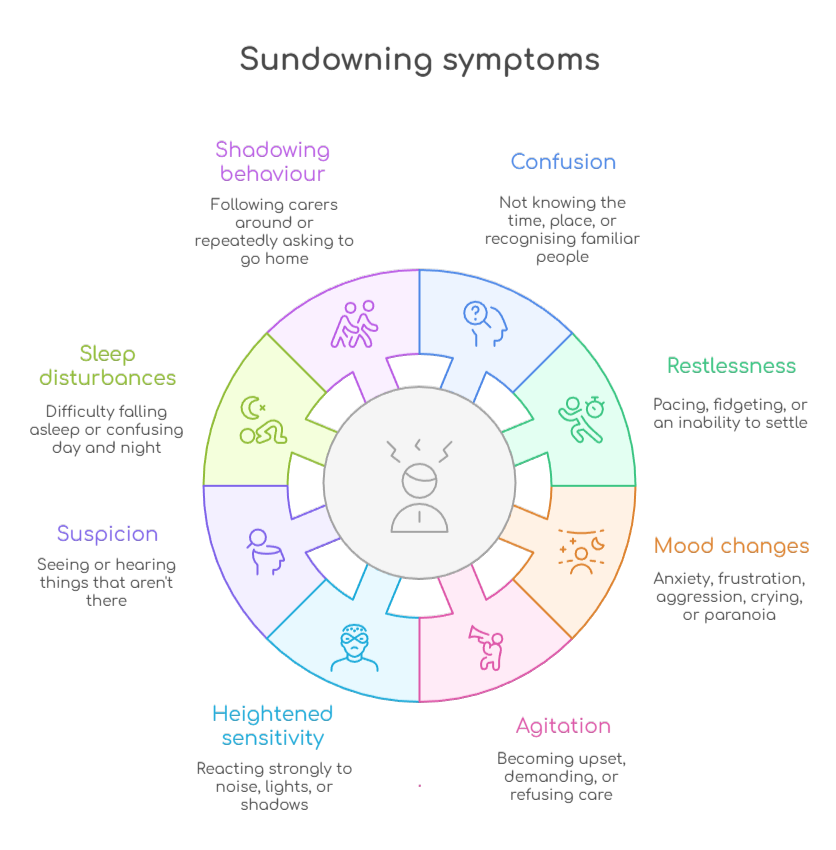
These symptoms can be distressing for both the person with dementia and their carers, especially when they happen daily or worsen over time.
Why does sundowning happen?
While the exact cause remains unclear, several contributing factors have been identified:
- Changes to the body clock
- Fatigue at the end of the day
- Environmental changes as daylight fades
- Unmet physical needs
- Overstimulation and routine disruption
- Illness or medication effects
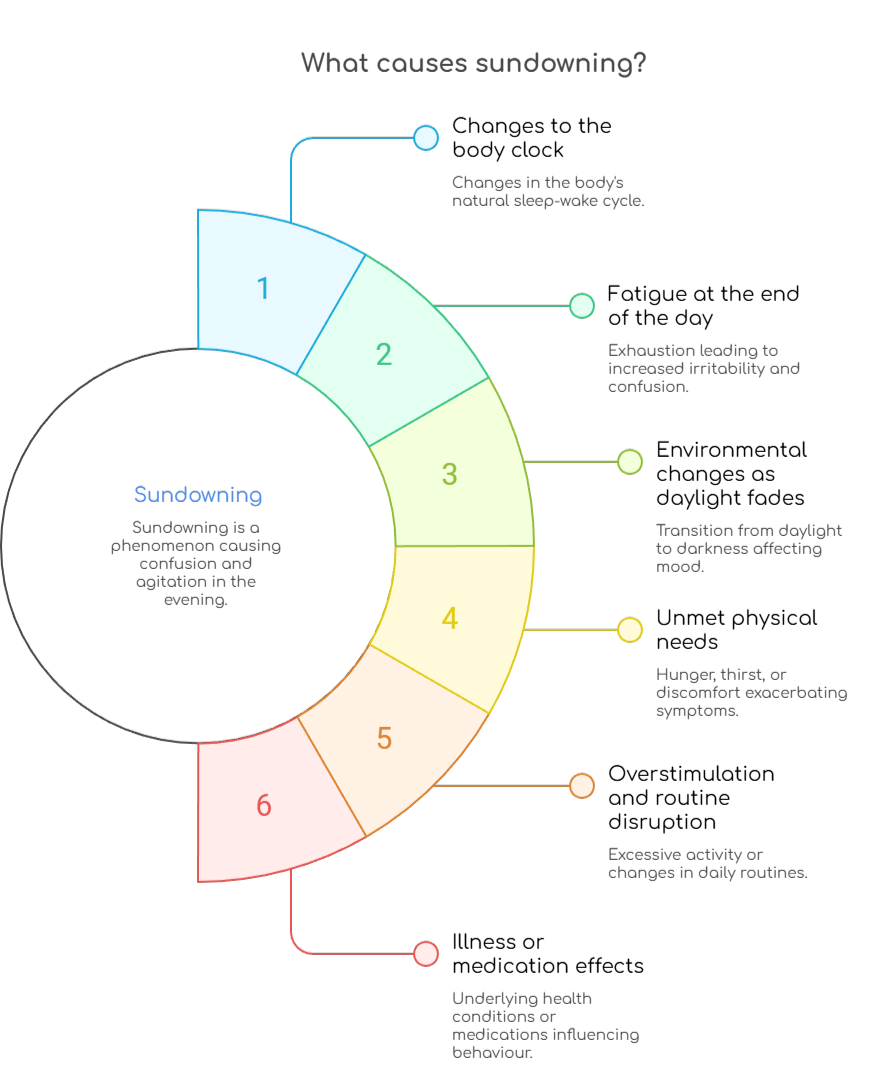
Changes to the body clock (circadian rhythm)
Dementia can affect brain areas that regulate the sleep–wake cycle. As this "internal clock" becomes less reliable, people can struggle to distinguish day from night, especially as the evening approaches.
This can lead to more wakefulness at night and more sleepiness during the day. Over time, this disrupted pattern can make late-day confusion and agitation more likely.
Fatigue at the end of the day
By late afternoon, many people with dementia have used up their mental and physical reserves. When the brain is tired, it becomes harder to cope with confusion, manage emotions, or tolerate stress.
Even small changes, like a slightly louder room or a missed snack, can feel overwhelming when the person is fatigued. This is why sundowning often appears after a busy day.
Environmental changes as daylight fades
Changing light can increase shadows and reduce visual cues. That can make ordinary spaces feel unfamiliar or threatening. As a result, it triggers fear, agitation, or misinterpretation.
People may also struggle more with depth perception in low light, which can make walking around the home feel unsafe. Closing curtains and turning lights on earlier can help reduce this effect.
Unmet physical needs
Hunger, thirst, needing the toilet, pain, constipation, or discomfort can all escalate sundowning. This is more often the case if the person can't clearly communicate what they need.
Discomfort may show up as pacing, calling out, or refusing care rather than a clear complaint. A quick check of basic needs in the late afternoon can prevent escalation.
Overstimulation and routine disruption
A busy day, visitors, noise, unfamiliar environments, or changes in routine can overwhelm someone with dementia. These occurrences make late-day agitation more likely.
Too much stimulation can build up across the day, then "spill over" in the evening when coping is lower. Keeping late afternoons quieter and more predictable often helps.
Illness or medication effects
Infections, dehydration, poor sleep, or medication side effects can worsen confusion and agitation. Sudden changes should always prompt a health check.
Sometimes sundowning-like behaviour is actually a sign of pain, infection, or a medication issue that needs treatment. If symptoms change quickly or feel out of character, it's worth speaking with a GP.
Practical management strategies for carers
Managing sundowning and dementia usually means reducing triggers and building a supportive environment. Try these strategies:
- Keep a consistent daily routine
- Optimise lighting throughout the day
- Balance activity and rest
- Reduce evening overstimulation
- Address basic physical needs
- Create a calm, familiar environment
- Track patterns and triggers
- Respond with patience and reassurance
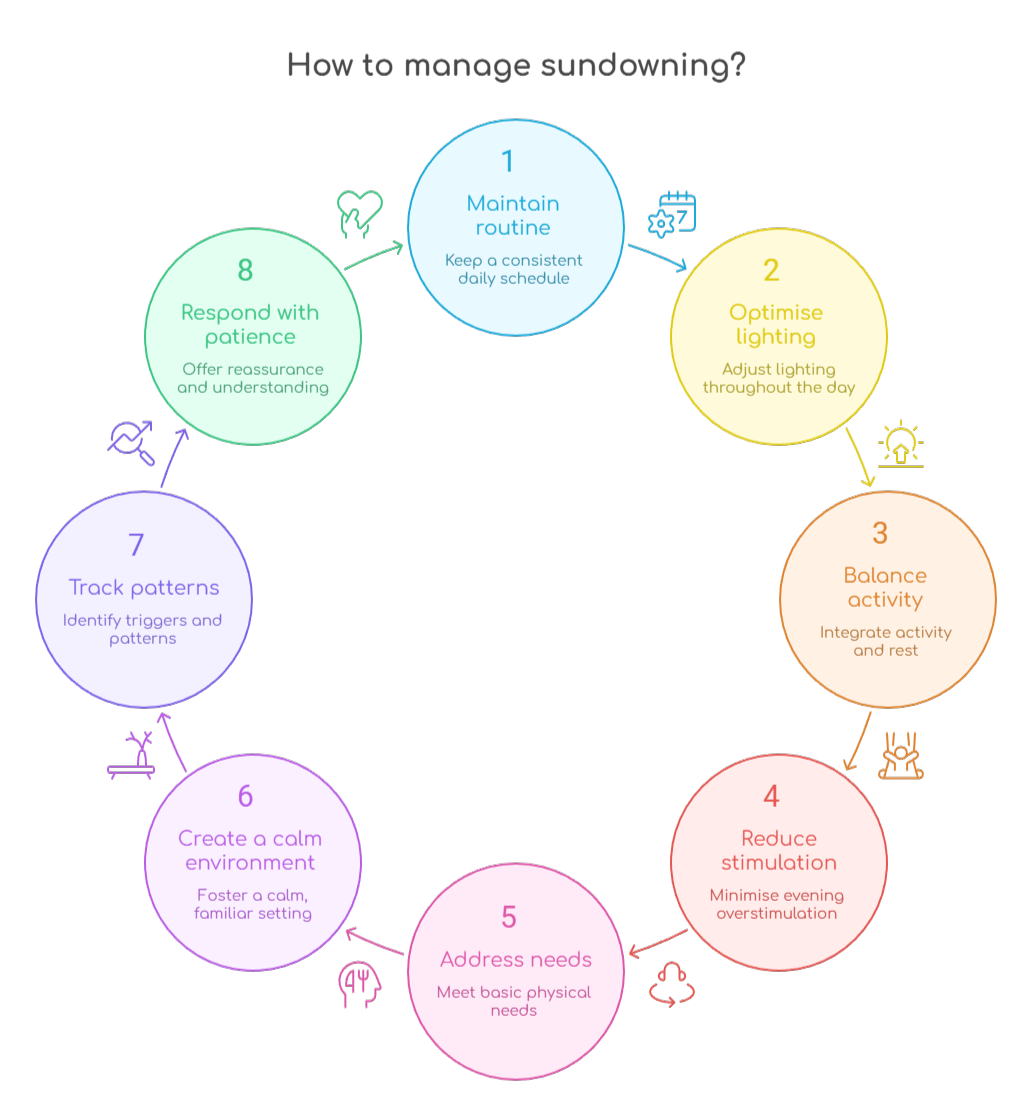
Keep a consistent daily routine
Predictability reduces confusion and anxiety. Keep regular times for waking, meals, and bedtime.
Avoid scheduling demanding tasks or appointments in the late afternoon when symptoms typically emerge.
If symptoms rise at a certain time, plan a calm transition beforehand. This can reduce stress during sundowning time.
Optimise lighting throughout the day
Use daylight to support orientation, which may include opening curtains and encouraging time outdoors when possible.
As evening approaches, turn on the lights before shadows form.
Use bright, even lighting to eliminate dark corners and shadows. Also, make sure to avoid glare from windows or harsh overhead lights.
Finally, consider leaving night lights on in hallways and bathrooms
Balance activity and rest
It's important to encourage gentle physical activity and social interaction in the morning or early afternoon.
Short walks and stimulating activities can also help, as long as they're not overwhelming.
Another helpful tip is to avoid long naps late in the day, as they can disrupt nighttime sleep. Instead, allow for rest periods earlier in the day if needed. This ensures the person isn't overtired by bedtime.
Reduce evening overstimulation
Late afternoon and evening should be calmer. This means you should limit noise, TV, and large gatherings at this time.
Avoid caffeine after midday, and offer a light snack instead of a heavy dinner.
It's vital to create a calm, quiet environment with soothing music or familiar activities. Also, make sure to minimise screens and stimulating activities before bed.
Address basic physical needs
Check regularly for hunger, thirst, pain, and discomfort to avoid sundowning. Also, encourage toilet visits before symptoms escalate.
Make sure clothing and room temperature are comfortable.
If needed, review medicines with a GP, as this can help rule out side effects.
Create a calm, familiar environment
Use familiar objects, photographs, or mementos that provide comfort. At the same time, maintain a clutter-free space that is easy to navigate.
You can also play soft music or engage in gentle, familiar activities like looking through photo albums.
Make sure to speak calmly and avoid arguing or correcting. If necessary, try distraction, like a short walk or a favourite snack.
Track patterns and triggers
Keep a diary noting when symptoms occur, what happened beforehand, and what helped.
This can reveal patterns that allow you to anticipate and prepare for sundowning episodes. You'll also be able to adjust care accordingly.
Respond with patience and reassurance
Remember that sundowning is not deliberate, and the person can't control these episodes.
As challenging as it may be, it's important to stay calm and validate feelings. This means avoiding confrontation.
Instead, reassure the person and focus on safety. Gentle redirection often helps more than logic.
When to seek medical advice
While sundowning is a common dementia symptom, it's important to consult a GP or specialist if:
- Symptoms suddenly worsen or change
- You suspect infection, pain, or medication side effects
- Behaviour creates safety risks for anyone
- You're struggling to manage at home
A doctor can assess for treatable causes and may suggest adjustments to medications or care strategies.
Support services for Australian carers
Caring for someone with sundowning can be exhausting. These Australian services can help:
- Dementia Australia
- My Aged Care
- Healthdirect
- Dementia pathways
- Local in-home care providers
Dementia Australia
Dementia Australia offers free resources, fact sheets, and support specifically addressing restlessness and sundowning.
Their National Dementia Helpline (1800 100 500) provides information, advice, support, and connections to local support groups and education programs.
You can also download guides tailored to Australian families.
My Aged Care
My Aged Care is the Australian Government's main entry point for accessing subsidised aged care.
Through My Aged Care, you can access government-funded services such as:
- Support at Home (this replaced Home Care Packages and Short-Term Restorative Care from 1 November 2025)
- Respite care to give carers a planned break
- Residential aged care if support needs are no longer manageable at home
- Assessments to confirm eligibility and the level of help needed
To get started, call 1800 200 422 or use the My Aged Care website.
Healthdirect
This government-funded service provides 24/7 nurse advice for health concerns. Call 1800 022 222 for immediate guidance or visit healthdirect.gov.au.
Dementia Pathways
This Australian resource offers free downloadable PDFs and tools for carers, including specific guidance on sundowning management.
Visit dementiapathways.com.au to access these materials.
Local in-home care providers
Many service providers across Australia offer specialised dementia care in the home. This includes support during challenging sundowning hours.
Contact My Aged Care for referrals to providers in your area.
How in-home support helps manage sundowning safely
Evenings are often the hardest time for carers, when sundowning time can peak. In-home support can reduce risk and pressure.
Support at Home can help with:
- Routine support in the late afternoon and evening (help with personal care, toileting, hydration, snacks, and settling for bed)
- Safer home setup (better lighting, fewer trip hazards, and calmer spaces)
- Dementia-informed reassurance (calm companionship can reduce anxiety and escalation)
- Wandering and safety support (extra supervision during higher-risk periods)
- Carer respite (a break for family carers, especially at the end of the day)
This support helps protect the person living with dementia and the well-being of carers.
FAQ
What are sundowners?
"Sundowners" is an informal term some people use. It refers to people who experience sundowning.
What time is sundowning?
Often late afternoon into the evening. The exact timing varies by person and day.
Is sundowning a stage of dementia?
No. Sundowning is a behaviour pattern that can happen at different stages, but it's often more noticeable as dementia progresses.
How long does sundowning last?
It varies. Some episodes last minutes, while others can continue for hours into the evening or night.
Does sundowning happen every day?
Not always. It may happen daily for some people. But for others, it comes and goes depending on triggers like fatigue, stress, or changes in routine.
Making sundowning safer and calmer
Sundowning can be one of the most challenging parts of dementia care, especially when it happens at the end of the day, and everyone is already tired.
Understanding what triggers sundowning behaviour and putting simple supports in place can reduce distress and improve safety.
If you're finding sundowning time hard to manage on your own, Sensible Care can help. We can provide in-home support to help evenings run more smoothly and give family carers a much-needed break.
With the right strategies and the right help, sundowning becomes more manageable, and home life can feel calmer again.
If you would like to know more, feel free to reach out to us.
Take the Next Step in Care
Download our Info Kit or speak to one of our friendly team members today.
Need Help Getting Started?
Reach out on your terms, pick a time that suits you and let’s talk about how we can help.
.webp)
.svg)