How does the Support at Home End-of-Life Pathway work?
Read on to learn how the Support at Home End-of-Life Pathway works in providing coordinated care, comfort, and support for people nearing the end of life.
Author: Sensible Care

The Support at Home End-of-Life Pathway offers urgent help to older Australians who have three months or less to live. It provides up to $25,000 in short-term funding for Support at Home. Funding can be used for nursing, personal care, and help around the house, alongside palliative care. Clinical services are fully government-funded, while other services may require a means-tested contribution.
Most Australians, when asked, say they'd prefer to die at home surrounded by loved ones.
Thanks to the Support at Home End-of-Life Pathway, this choice has become more accessible for older Australians with limited time remaining.
This pathway is designed for older people who have been told they may have three months or less to live. It provides short-term funding for additional help at home when it's most needed.
In this guide, we'll explain who can access this pathway, what it covers, and how to apply. We'll also outline likely costs, what happens when the funding ends, and how to access extra support.
What is the End-of-Life Pathway?
The End-of-Life Pathway is a high-priority, short-term support option under Support at Home. It's for people who have about three months or less to live, and want to stay at home for the time that remains.
It provides around $25,000 in funding, which can be used for approved Support at Home services.
This pathway typically lasts 12 weeks, but patients can continue using any remaining funds for up to 16 weeks.
Funding covers practical day-to-day supports, such as personal care, nursing, domestic help, and respite. It's designed to work alongside palliative care you may already be receiving through your state or territory.
This pathway does not replace your doctor or palliative care team. It funds practical, everyday help that can make staying at home possible when your health declines.
Who is eligible?
You may be eligible for the Support at Home End-of-Life Pathway if you meet medical and age criteria and wish to remain at home.
To apply, your doctor or nurse practitioner must also complete the End-of-Life Pathway form.
Eligibility includes:
- Prognosis: A doctor or nurse practitioner must confirm an estimated life expectancy of three months or less.
- Age: You must meet the age requirement, which is typically 65+ (50+ for Aboriginal and Torres Strait Islander people).
- Location: You must prefer to remain at home rather than move to a residential aged care facility or a hospital.
- Documentation: Your clinician confirms you are in bed more than half the day (AKPS, Australian-modified Karnofsky Performance Status, score 40 or lower).
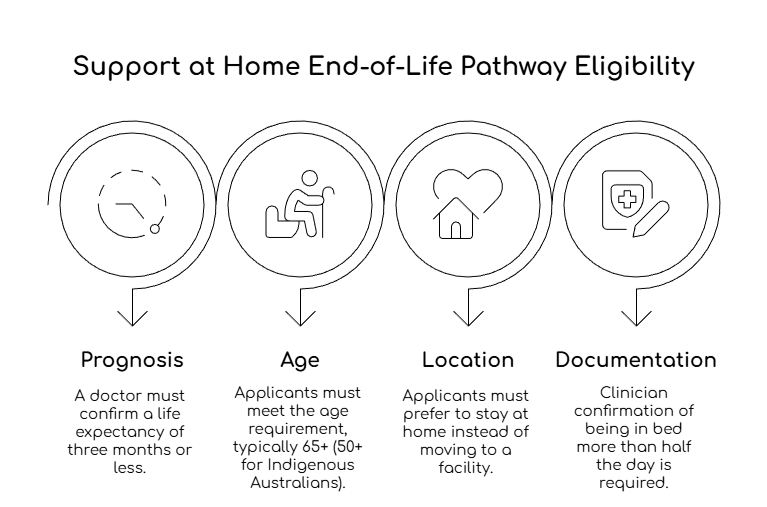
Note that you don't need to already be enrolled in Support at Home services. The pathway offers urgent priority access specifically for end-of-life care.
If you're already receiving Support at Home, your provider can request an urgent review to access the pathway.
What services does the $25,000 cover?
Your support plan is meant to be flexible, based on what you need most at the moment. Funding can also be used for assistive technology where needed.
Support at Home groups services into three categories:
- Clinical supports (health care services like nursing and physiotherapy) have no contribution, because the government pays 100%.
- Independence supports (help with personal tasks like showering) may require a contribution, depending on your means assessment.
- Everyday living supports (help at home, like cleaning and gardening) may require a higher contribution, depending on your means assessment.
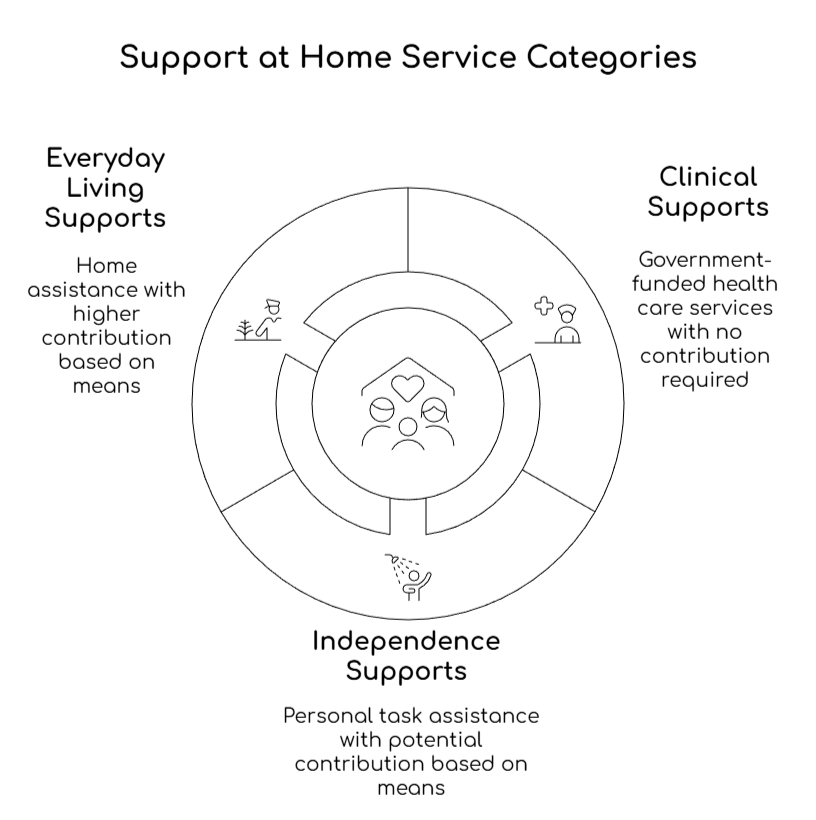
Clinical supports are fully government-funded. However, you may need to contribute to independence and everyday living services. Your contributions will be based on a means-tested assessment.
This pathway also coordinates with free specialist palliative care services provided by your state or territory health system. These teams manage complex symptoms like:
- Pain
- Breathing difficulties
- Anxiety through doctor visits
- Specialist nursing
- 24/7 phone support
How to access the Support at Home End-of-Life Pathway
The application process is fast, recognising the urgency when someone has limited time. This is what it involves:
- Medical assessment: Your GP or nurse practitioner completes the End-of-Life Pathway form, confirming your prognosis.
- Requesting a priority assessment: Contact My Aged Care (or apply online) or visit an Aged Care Specialist Officer at a Services Australia centre.
- Rapid assessment: An assessor will conduct a comprehensive home-based assessment (typically 1-3 hours) to determine your needs and create a support plan.
- Notice of Decision: This outlines your funding and approved services.
- Choose a provider: Select an aged care provider from the My Aged Care portal (if you're already with a provider, staying with them avoids delays).
- Services begin: Your provider arranges care delivery, typically starting within days.

This pathway prioritises urgent cases to minimise waiting times. This marks an important difference from standard aged care assessments, which can take weeks or months.
Understanding costs and contributions
Clinical supports have no participant contribution. Independence and everyday living services may involve a contribution, based on your income and assets.
The Department's standard contribution rates from 1 November 2025 include:
- Full pensioner: 5% for independence services, and 17.5% for everyday living services.
- Part pensioner or eligible Commonwealth Seniors Health Card holder: 5%–50% for independence, and 17.5%–80% for everyday living.
- Self-funded retiree: 50% for independence, and 80% for everyday living.
There is also a lifetime cap on contributions:
- Standard lifetime cap: $135,318.69 (indexed as of 20 September 2025).
- If the "no worse off principle" applies (a rule that protects existing clients), the cap is $84,571.66 (indexed as of 20 September 2025).
On average, the government contributes about $7.80 for every $1 a person contributes to Support at Home.
Preparing for end-of-life care at home
Good planning reduces stress for everyone. Your GP and palliative care team can help you create a clear plan for support, symptoms, and after-hours contacts.
Practical preparations to consider:
- Ask about equipment needs, such as a hospital bed, and who can organise them.
- Plan carer support, including who can stay overnight if needed.
- Ask your care team what to do if distressing symptoms occur suddenly, especially outside of regular business hours.
It's also helpful to have some planning documents ready. These may include:
- An advance care directive (a written record of care wishes) can guide decisions if the person is unable to speak for themselves.
- A substitute decision-maker document, such as an enduring power of attorney, can help with health and financial decisions.
What happens after 16 weeks?
The End-of-Life Pathway funding lasts up to 16 weeks total (12 weeks standard, extendable if funds remain).
If you're still living at home beyond this period:
- Your provider can request a high-priority Support Plan Review to transition you to ongoing Support at Home services.
- You'll receive a new funding allocation based on your ongoing care needs (classified into levels 1-8).
- Your existing services can continue without interruption during the transition.
The $25,000 replaces any other My Aged Care funding during the pathway period. But it doesn't count toward the lifetime contribution cap of $84,572 for ongoing Support at Home services.
What to do when death occurs at home
If the death is expected and the person was receiving palliative care at home, you usually do not need to call emergency services. You can contact the person's doctor or palliative care team, and there is often no rush.
This is what you can do:
- Call the GP or palliative care team when you are ready, so they can arrange the medical certificate.
- Take the time you need, as the person can stay at home for a few hours if you wish.
- Contact your chosen funeral director when you are ready, and they will guide you through the next steps.
If the death is unexpected, or you are unsure what has happened, call 000 and follow their instructions.
If you are considering the pathway
The Support at Home End-of-Life Pathway is designed to reduce stress when time is limited. It provides short-term funding and urgent access to practical help at home. For many people, that support can make the difference between staying home and needing hospital care.
If you or someone you care for wants to remain at home in their final months, start by consulting your GP or treating team. Ask whether the End-of-Life Pathway form is appropriate, and what to do next.
If you want help putting the End-of-Life Pathway into action, Sensible Care can support you through the process. We can talk through your needs, help you understand your options, and organise the services that make staying at home more manageable.
Contact Sensible Care today to discuss urgent home support and next steps.
Take the Next Step in Care
Download our Info Kit or speak to one of our friendly team members today.
Need Help Getting Started?
Reach out on your terms, pick a time that suits you and let’s talk about how we can help.
.webp)
.svg)
.webp)

